Research Explained: OCNDS core features are conserved across variants, with loop-region mutations driving greater symptom burden
Authors: Elena Bagatelas, Maahin Manzoor Khan, and Gabrielle V. Rushing
Written by: Elena Bagatelas, CSNK2A1 Foundation Intern and Gabrielle Rushing, PhD, Chief Scientific Officer, CSNK2A1 Foundation
Link to Publication: https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1589897/full
Helpful Definitions:
- Phenotype: The traits or symptoms you can see or measure in a person.
- Missense variant: A change in a gene that swaps one building block in a protein for another. This can change how the protein functions.
Disclaimer:
This study focuses specifically on individuals with missense variants in the CSNK2A1 gene. These are changes that alter a single building block in the resulting protein. Other types of variants (such as nonsense, deletions, frameshift, or splice-site changes) were not included in this analysis, so the findings may not apply to all individuals with OCNDS.
Research Explained Summary
In this study, researchers at the CSNK2A1 Foundation looked at 48 people with OCNDS to understand how changes in different parts of the CSNK2A1 gene (called missense variants) affect symptoms. This gene makes a protein called CK2α, which helps regulate many important processes in the brain and body.
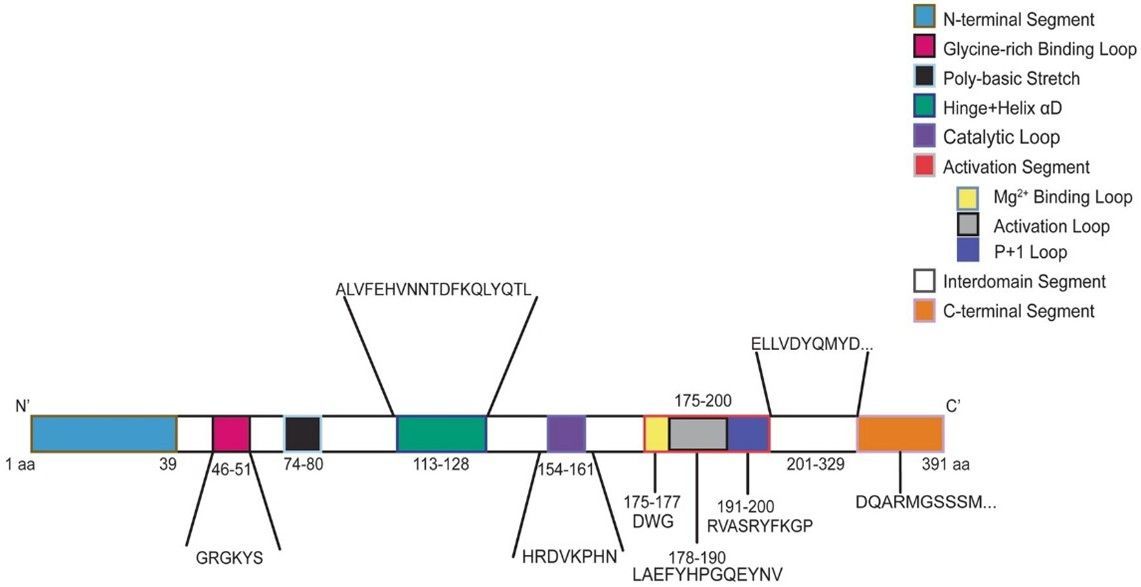
The researchers grouped individuals based on where their genetic changes occur in the protein’s structure. Some were in special “loop” regions which are important for protein function and others were outside those regions. They found that over half of the group had changes in two specific loops: the P+1 loop and the Glycine-rich loop, which have been shown to be critical structures for the protein in other studies. This figure shows the CK2 protein with the segments labeled:
People with changes in the loop regions tended to have more symptoms reported by families and doctors, reported as a higher symptom burden. For example, they were more likely to have low muscle tone (hypotonia) and were often diagnosed with OCNDS at a younger age.
However, a higher symptom burden does not always mean a person is more severely affected meaning that everyone with OCNDS is different, and having more symptoms doesn’t always mean they’re more affected. We also still don’t fully understand how symptoms change over a person’s lifetime. That’s why it’s so important to keep studying OCNDS, especially as individuals grow into adolescence and adulthood. Across the whole group, there were several common features:
- Speech and language delays were present in all 100% of the individuals.
- About ≥50% had trouble sleeping, neurological symptoms, constipation, global developmental delay, hormone-related (endocrine) issues, and vision problems.
- 82% met the cutoff for a pediatric sleep disorder, showing how serious and common sleep difficulties are in OCNDS.
This study helps researchers define a “core set” of symptoms such as sleep issues, constipation, and speech and language delays, that are especially important to target in future treatments. It also shows that we need better tools to measure how OCNDS affects everyday life, such as clinical severity and quality-of-life scales made specifically for this condition.
This paper was possible using data from Simons Searchlight. Your participation in the Simons Searchlight natural history study is what makes studies like this possible. The more individuals who take part, the more robust and meaningful the findings become. Each person’s experience helps build a clearer picture of OCNDS and brings us closer to discovering the best ways to support and treat this condition.
