Family Planning and Reproductive Options for Families with Okur-Chung Neurodevelopmental Syndrome
Authored by: Anna Madden, Master's Student in the Genetic Counseling Program at the University of Pennsylvania
Edited by: Gabrielle Rushing, PhD, CSNK2A1 Foundation Chief Scientific Author & Jennifer Sills, CSNK2A1 Foundation Founder and President
Understanding the likelihood of having another child with Okur-Chung Neurodevelopmental Syndrome (OCNDS) depends on whether the CSNK2A1 genetic variant is present in either biological parent.
The following guide explains to help you understand the chances of recurrence based on a sample genetic testing report.
1. If Your Child’s Report Says “De Novo”
| Gene | Condition | Mode of Inheritance | Variant | Coding DNA | Zygosity | Inherited From | Classification |
|---|---|---|---|---|---|---|---|
| CSNK2A1 | Okur-Chung Neurodevelopmental Syndrome | Autosomal Dominant | p.R47G | c.139 C>G | Heterozygous | De Novo | Pathogenic Variant |
What does "de novo" mean?
- A “de novo” variant means the genetic change was found new in your child and WAS NOT PASSED DOWN from either parent.
What does this mean for future pregnancies?
- The likelihood of having another child with OCNDS is about 1%
Why the 1%?
- While the sample used for testing (typically blood or saliva) does a good job of detecting the CSNK2A1 variant, the sample doesn’t always represent every cell in the body. There is a small chance that the genetic variant could be present in a parent’s egg or sperm cells and could be passed onto another child, even if it wasn't found in the parent’s sample. We say the chance of this happening is about 1% or 1 out of 100.
2. If Your Child’s Report Says Inherited From “Maternal” or “Paternal”
| Gene | Condition | Mode of Inheritance | Variant | Coding DNA | Zygosity | Inherited From | Classification |
|---|---|---|---|---|---|---|---|
| CSNK2A1 | Okur-Chung Neurodevelopmental Syndrome | Autosomal Dominant | p.R47G | c.139 C>G | Heterozygous | Maternal | Pathogenic Variant |
What does this mean?
- This indicates that the genetic variant was found both in your child and in either the mother or father.
What does this mean for future pregnancies?
- The likelihood of having another child with OCNDS is 50% for each additional pregnancy. This means that each time a couple gets pregnant, there is a 50% chance of having another child with OCNDS.
- It’s important to know that this 50% chance of passing on the variant does not mean that 50% of a given couple’s children will be affected with OCNDS. One helpful way to think about this is to compare the chance of inheriting or not inheriting the variant to a coin flip, where there is a 50% chance of landing on heads and a 50% chance of landing on tails with each toss. You might flip a coin four times and they are all heads, all tails, or any number in between. Likewise, if a couple has 4 children, this does not mean that exactly half of their children, or 2 in this case, will be affected. They may by chance have four affected children, none affected, or any number in between.
Why the 50%?
- We all have two copies of each gene in our bodies — one inherited from each of our parents. OCNDS is an autosomal dominant condition, which means that having one altered copy of the CSNK2A1 gene is enough to cause the condition.
- When a parent carries a CSNK2A1 variant, they have one altered copy of the gene with the variant and one working copy. When that parent has a child, they can pass down either the altered copy or the working copy of the gene.
- Therefore, the child has a 50% chance of inheriting the altered copy and thus developing OCNDS, and a 50% chance of inheriting the working copy and being unaffected.
| Gene | Condition | Mode of Inheritance | Variant | Coding DNA | Zygosity | Inherited From | Classification |
|---|---|---|---|---|---|---|---|
| CSNK2A1 | Okur-Chung Neurodevelopmental Syndrome | Autosomal Dominant | p.R47G | c.139 C>G | Heterozygous | Maternal | Pathogenic Variant |
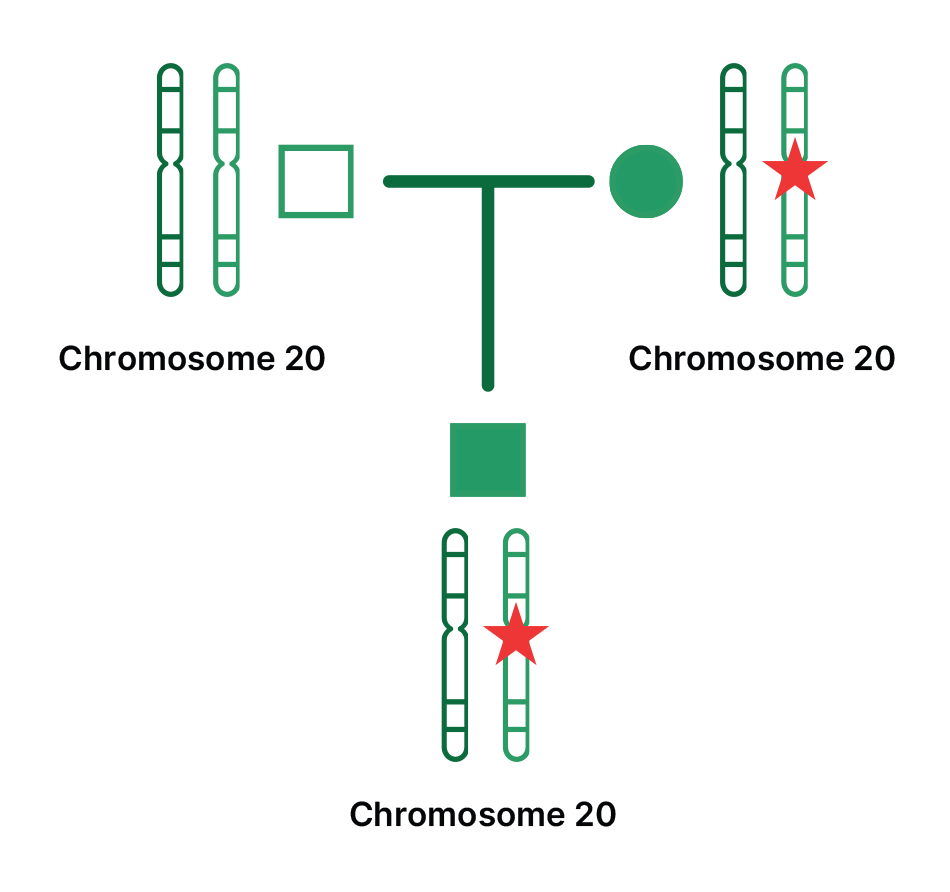
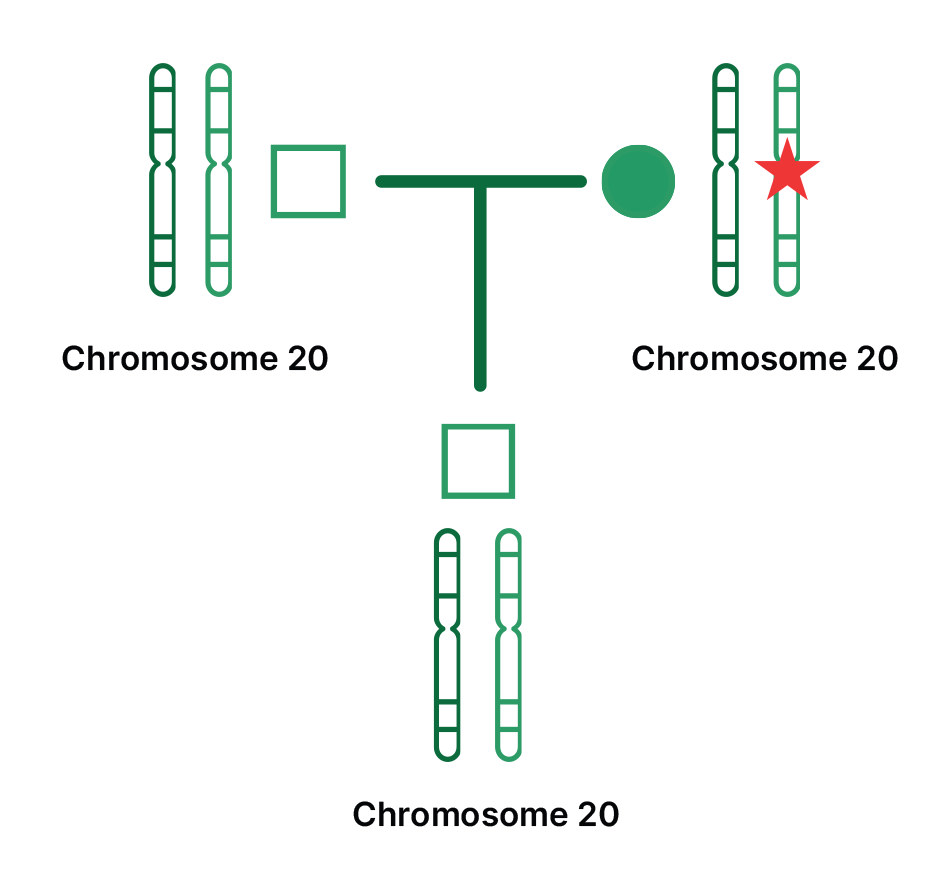
THE DIAGRAMS BELOW SHOW HOW A CHILD CAN EITHER INHERIT THE ALTERED OR WORKING COPY FROM A PARENT.
Males are shown as squares and;
Females are shown as Circles.
The star represents a genetic variant on chromosome 20, the chromosome involved in OCNDS.
Parents are connected by horizontal lines with their child shown below them.
Here, the child inherited the altered copy of chromosome 20 from their mother, as shown by the stars. This child has OCNDS.
Here, the child DID NOT inherit the altered copy of chromosome 20 from their mother. This child does not have OCNDS.
Reproductive Options for Families with OCNDS
Note: This guidance is based on practices in the United States and may not reflect genetic testing practices, healthcare systems, or reproductive options available in other countries. Families outside of the United States should consult with a local healthcare provider (or genetic counselor if available) to understand the options and services available in their region.
1. Prenatal Testing:
In certain countries like the United States, prenatal testing can be performed during pregnancy to determine if the fetus carries a genetic variant linked to OCNDS. This type of testing is typically considered if one of the parents or a previous pregnancy is known to carry a genetic variant associated with OCNDS. If there is no family history of the condition, OCNDS is not routinely screened or tested for during pregnancy. Common prenatal testing methods for pregnancies when there is a known family history of the condition include:
- Chorionic Villus Sampling (CVS): A procedure to obtain a sample of tissue from the placenta, typically performed between 10 and 13 weeks of pregnancy.
- Amniocentesis: A procedure where a small amount of amniotic fluid is taken for testing, typically starting at 15 weeks of pregnancy.
2. Preimplantation Genetic Testing (PGT):
For families undergoing in vitro fertilization (IVF), preimplantation genetic testing (PGT) may be available in certain countries. PGT can be used to screen embryos for the genetic variant associated with OCNDS before they are implanted in the womb. This option enables families to select embryos that do not carry the variant associated with OCNDS, which may have been identified in a previous family member. If a parent is known to carry the genetic variant associated with OCNDS, PGT can help select embryos that have not inherited the variant. Policies on offering PGT can vary between laboratories and countries, especially when a previous child is found to have a de novo genetic change that was not present in either parent. You can discuss the possibility of PGT with your healthcare provider or genetic counselor for more details.
3. Genetic Testing After Birth:
Instead of testing during the pregnancy, genetic testing can be performed after birth, especially if the child has symptoms of OCNDS.
4. Egg or Sperm Donation:
If one parent is affected by OCNDS and wishes to reduce the likelihood of passing the variant on to their child, egg or sperm donation from an unaffected donor can be considered as an option.
5. Adoption:
Adoption is an option for families who are concerned about having another child with OCNDS.
6. Declining Genetic Testing in Future Pregnancies:
Some families may choose not to undergo genetic testing in future pregnancies. This choice may be based on personal values, comfort with uncertainty, or a decision to prepare for and support the child regardless of genetic status.
7. Choosing Not to Pursue Additional Pregnancies:
Some families, after learning about chance of having another child with OCNDS, may decide not to pursue additional pregnancies. This is a deeply personal decision that can be informed by many factors, including emotional, financial, and medical considerations.
8. Genetic Counseling:
Consulting with a genetic counselor can help families talk through these options and answer any questions.
